Connect With Us
Blog
Items filtered by date: December 2021
Foot Structure May Change During Pregnancy

Pregnancy brings about a multitude of changes in a woman's body, and one area that is often overlooked is the feet. Throughout pregnancy, hormonal fluctuations, weight gain, and shifts in the body's center of gravity can significantly impact foot structure. As the body produces hormones like relaxin to loosen ligaments in preparation for childbirth, the arches of the feet may flatten, leading to a condition known as overpronation. This change in foot posture can cause discomfort, instability, and increased strain on the ankles and knees. Additionally, swelling, or edema, commonly experienced during pregnancy can add to foot-related issues. Proper footwear with adequate support and cushioning becomes essential to alleviate discomfort and maintain stability. Regular foot care, including gentle stretching exercises and elevation to reduce swelling, can help diminish the effects of these structural changes. If your feet are uncomfortable during your pregnancy, or you have developed foot pain, it is suggested that you speak to a podiatrist who can help you to find relief.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with the foot specialists from Affiliates in Foot Care, P.C.. Our doctors will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions please feel free to contact our office located in Woburn, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Do Your Child's Feet Hurt?
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Treatment for Flat Foot
 Flat foot, which occurs when the foot's arch collapses, can lead to discomfort and pain, particularly in the heel or arch area. This condition may also affect overall foot function. To manage and treat flat feet, a podiatrist might recommend several supportive therapies depending on the severity of the condition and the specific needs of the patient. One common treatment is the use of arch support insoles, which are inserts for the shoes. These insoles help to distribute pressure more evenly across the foot, provide stability, and relieve strain on the arch and surrounding muscles. For cases where insoles alone are not sufficient, a podiatrist may also suggest additional support through structured shoes with built-in arch support, ankle braces, or foot orthotics. Severe cases may require corrective exercises or even surgery to realign the foot and restore function. Regular monitoring and adjustments by a podiatrist are important to effectively manage flat foot and prevent further complications. If you have a flat foot, it is suggested that you make an appointment with a podiatrist.
Flat foot, which occurs when the foot's arch collapses, can lead to discomfort and pain, particularly in the heel or arch area. This condition may also affect overall foot function. To manage and treat flat feet, a podiatrist might recommend several supportive therapies depending on the severity of the condition and the specific needs of the patient. One common treatment is the use of arch support insoles, which are inserts for the shoes. These insoles help to distribute pressure more evenly across the foot, provide stability, and relieve strain on the arch and surrounding muscles. For cases where insoles alone are not sufficient, a podiatrist may also suggest additional support through structured shoes with built-in arch support, ankle braces, or foot orthotics. Severe cases may require corrective exercises or even surgery to realign the foot and restore function. Regular monitoring and adjustments by a podiatrist are important to effectively manage flat foot and prevent further complications. If you have a flat foot, it is suggested that you make an appointment with a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact the foot specialists from Affiliates in Foot Care, P.C.. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Woburn, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Get a Proper Shoe Fit
Many people suffer from foot problems because their shoes are poorly fitted. When shopping for a new pair of shoes, fashion usually triumphs over comfortability. A pair of well fitted shoes is essential in preventing foot problems and potential injuries.
Poorly fitted shoes can cause foot issues such as plantar fasciitis, bunions, hammertoes, ingrown toenails, and foot pain. Shoes such as high heels and sandals may cause problems for your feet. These shoes put the foot in an unnatural position for long periods and fail to provide good foot support. It is recommended to not wear either one for an extended period.
When you are trying on shoes, make sure they have enough space for your toes to move around. Shoes shouldn’t be cramped but also shouldn’t have too much room that your foot moves around in them. A snug shoe is a good choice. They should also provide good arch support and cushioning. Athletic shoes tend to offer both good support and cushioning. A degree of flexibility is necessary so they aren’t too stiff or too unsupportive.
If you can wear your shoes for a long period of time without experiencing any discomfort, this is a sign that your shoes fit properly. Do not be too dismayed if the shoe isn’t a perfect fit at first; many shoes take a few days to weeks to properly break in. However don’t expect an uncomfortable shoe to become fitted to your foot.
For those with foot conditions such as flat feet or pronation, orthotics may be helpful or even necessary to prevent foot pain. Orthotics are inserts that are placed in the shoe and provide support and cushioning for the foot. While there are many types of orthotics out there, custom-made orthotics may be necessary depending upon your foot and foot conditions.
Feet change in size over time. It is important to check your foot size over time so that you can make sure you have the perfect fit for your feet. A podiatrist can provide more information on proper shoe fitting and foot orthotics.
How to Make Sure Shoes Fit Well

Ensuring your shoes fit properly is critical for comfort and foot health. Begin by measuring your feet later in the day when they are at their largest, and stand while measuring to mimic weight-bearing conditions. Take note of both length and width, including the arch length, as this affects shoe fit. Keep in mind that sizes can vary between shoe brands, so always prioritize fit over the number on the label. If your feet are different sizes, opt for the larger size to prevent discomfort. During fitting, wear the same type of socks or foot coverings you plan to wear with the shoes. Leave a thumb's width of space at the front and back of the shoes to accommodate natural foot swelling and movement. For personalized advice and to address any specific concerns, it is suggested you schedule an appointment with a podiatrist who can offer you invaluable guidance.
It is important to find shoes that fit you properly in order to avoid a variety of different foot problems. For more information about treatment, contact the foot specialists from Affiliates in Foot Care, P.C.. Our doctors will treat your foot and ankle needs.
Proper Shoe Fitting
Shoes have many different functions. They cushion our body weight, protect our feet, and allow us to safely play sports. You should always make sure that the shoes you wear fit you properly in order to avoid injuries and deformities such as: bunions, corns, calluses, hammertoes, plantar fasciitis, stress fractures, and more. It is important to note that although a certain pair of shoes might be a great fit for someone else, that doesn’t mean they will be a great fit for you. This is why you should always try on shoes before buying them to make sure they are worth the investment. Typically, shoes need to be replaced ever six months to one year of regular use.
Tips for Proper Shoe Fitting
- Select a shoe that is shaped like your foot
- Don’t buy shoes that fit too tight, expecting them to stretch to fit
- Make sure there is enough space (3/8” to ½”) for your longest toe at the end of each shoe when you are standing up
- Walk in the shoes to make sure they fit and feel right
- Don’t select shoes by the size marked inside the shoe, but by how the shoe fits your foot
The shoes you buy should always feel as good as they look. Shoes that fit properly will last longer, feel better, and improve your way of life each day.
If you have any questions, please feel free to contact our office located in Woburn, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
Facts About Bunion Surgery

Bunion surgery, known as a bunionectomy, is a common procedure aimed at correcting the misalignment of the big toe joint caused by a bony bump known as a bunion. While bunion surgery can provide relief from pain and improve foot function, it is essential to understand several key facts before undergoing the procedure. Firstly, there are different types of bunion surgeries, ranging from minimally invasive techniques to more extensive procedures depending on the severity of the bunion and individual patient factors. Secondly, recovery from bunion surgery typically involves a period of immobilization followed by exercises to restore strength and flexibility to the foot. Additionally, it is important to have realistic expectations about the outcome of bunion surgery, as full recovery can take several months, and there may still be some residual stiffness or swelling afterward. If you have a bunion and are considering surgery, it is strongly suggested that you seek advice from a podiatrist who can determine if this is a right decision for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact the foot specialists of Affiliates in Foot Care, P.C.. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Woburn, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
The Progression of Foot Ulcer Stages
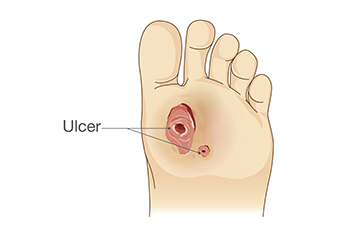
Foot ulcers, a common complication among individuals with diabetes or circulatory issues, undergo distinct stages as they develop and heal. These stages offer insights into the severity of the ulcer. Podiatrists can use the stages as a guide for treatment decisions. Initially, ulcers may start as redness or irritation on the skin, indicating early-stage ulcer formation. As the condition progresses, the ulcer may deepen, forming an open sore or wound. At this stage, infection becomes a significant concern that requires prompt medical attention to prevent complications. Without proper treatment, ulcers can advance to deeper tissue layers, exposing tendons, bones, or joints. This stage poses a heightened risk of severe infection and potential limb loss, underscoring the importance of vigilant wound care and regular monitoring. If you are diabetic and you develop a foot wound, it is strongly suggested that you are under the care of a podiatrist who can provide you with proper wound care treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with the foot specialists from Affiliates in Foot Care, P.C.. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Woburn, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.